PRP/ Stem Cell Therapy
Platelet Rich Plasma (PRP) therapy and Bone Marrow Aspirate Concentrate (BMAC) are relatively new treatments designed to aid in the healing and regeneration of soft tissues such as tendons and ligaments as well as joint structures. To fully understand the benefits of these therapies, it is first useful to have some understanding of the basic science behind tendon and ligament injuries.
Tendons and ligaments are made up of fibers of collagen. When these fibers are stretched or torn we may refer to the injury as a “pull”, “tear”, “sprain” (ligament) or “strain” (tendon). These structures are vascular, which means there are blood vessels in them. Thus, when they are injured they bleed. If there is enough bleeding we may notice bruising around the area of injury. Blood flow to the area increases to aid in healing. The blood carries platelets and growth factors that allow for healing of the tissue by creating new collagen fibers. These new fibers need to be constructed in an organized, layered fashion to heal correctly and allow the structure to regain its proper strength and flexibility.
Sometimes, the healing process does not work correctly and instead of forming healthy collagen fibers, significant scar tissue develops in its place. One of the risk factors is not getting enough blood flow to the area to provide those platelets and healing factors. The development of scar tissue further prohibits proper blood flow, as new small blood vessels can’t penetrate through the scar tissue to provide blood flow to the injured area. The new development of small blood vessels is called “angiogenesis” or “neovascularization”. When scarred or disorganized tissue inhibits this process, the blood flow to the area becomes “blocked”. This means that the tissue will never really have the opportunity to heal correctly. That is why sometimes ligament and tendon injuries heal while at other times they don’t.
When these injuries don’t heal, patients often become frustrated. They may try anti-inflammatories and other pain medications, topical creams, gels, braces, physical therapy, massage, acupuncture and cortisone injections, but nothing seems to work. That’s because these therapies may try to treat pain and inflammation but they don’t treat the underlying problem of scar tissues, which is disordered fibers and poor angiogenesis (blood flow). The result is many patients may give up and live with pain and disability, or may end up with surgery.
PRP and/or BMAC therapy may help this problem. In PRP treatment the patient’s own blood is taken with a simple blood draw. Using a special centrifuge machine, this blood is spun down. The process separates out and concentrates the platelets and growth factors that are essential for healing. This small amount of fluid with concentrated platelets and growth factors is called platelet rich plasma (PRP). Nothing else is added to your blood, so there is no risk of allergy, reaction or rejection. PRP therapy is a purely natural process, using your body’s own healing factors.
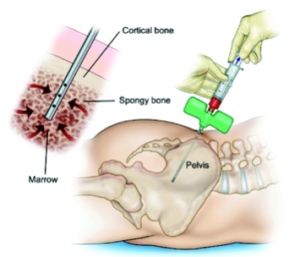
BMAC involves the aspiration of cells and growth factors from the bone marrow. In most cases, we aspirate the area of the iliac crest, using ultrasound guidance after thoroughly numbing the area with a local anesthetic, so that it is relatively painless. The process is very similar in that we take the cells from the area of the iliac crest and concentrate these cells using a centrifuge. The concentrated cells are then injected into the area.
PRP, which contains growth factors spun down from whole blood, is not a stem cell product and may contain a few cells responsible for stimulation. Therefore, PRPis not really a stem cell product.
Because bone marrow (BMAC) consists of greater than 90% whole blood, there is nothing in PRP that isn’t in the bone marrow in greater quantities. The biggest distinction is that bone marrow contains mesenchymal stem cells and other types of stem cells. PRP does not. PRP has been shown to speed up repair, but bone marrow aspirate may do it faster. Basically, anything that PRP does, BMAC does better, but PRP can be used as a cheaper stopgap alternative for inflammatory problems. However, if economics were not a concern, then BMAC would be the ideal choice.
As opposed to PRP, which contains only growth factors and very few cells, BMAC contains a mix of stem and progenitor cells, platelets and white blood cells—each making their own contribution to the healing process. Stem cells can differentiate into many different types of cells. There are several types of stem cells, including hematopoietic and mesenchymal. They vary in differentiation potential and the terminal cell types they can become. Hematopoietic stem cells (HSCs) typically differentiate into blood and vasculature cell components. Mesenchymal stem cells (MSCs) have the capability to differentiate into many different cell types responsible for repair or growth of bone, cartilage, muscle, marrow, tendons, ligaments and connective tissue. BMAC delivers a highly concentrated sample of stem cells, progenitor cells and growth factors directly to the application site, harnessing the body’s biologic potential.
Once the material is concentrated, the trick is getting ANY of these cells and factors to the right place!
We then use a diagnostic ultrasound machine to identify the area within the ligament, joint or tendon that is injured. The newest ultrasound technology provides resolution to see every millimeter of the collagen fibers as well as scar tissue and blood flow to the area. We then use a needle to inject the PRP directly into the injured area. The PRP can even be injected directly into very small tears that are sometimes not apparent on MRI. Once these platelets and growth factors are in the area of injury, they become activated. They also recruit other healing proteins and factors to the area and healing and regeneration of the tissue can now begin.
This therapy has been used extensively in Europe for several years and is now becoming more popular in the U.S. as more people become aware of its potential benefits. However, the idea of getting blood to an injured area is not new. For years, many people have tried needling tissue or even injecting an irritant into the tissue (prolotherapy) to attempt to increase blood flow to the injured area. Now with the development of PRP we can actually get the specific healing factors within the blood to the injured area. This not only allows for healing of injuries that may not otherwise heal, but it also speeds up recovery of injuries that may eventually heal over a longer period of time. Thus, PRP therapy is a great option for two different patient populations. One is group with chronic injuries that never seem to go away. The other is the patient with an acute injury that might otherwise take 8-12 weeks to heal and is looking to do something to “speed up” the recovery process. That is why PRP has become so popular among athletes. There have been many media reports of elite athletes receiving PRP treatment for injuries that occur mid-season or even right before big events, such as the Superbowl. But PRP treatment is not just for athletes.
These therapies can be used with great success in many conditions including:
Acute and chronic tendon injuries (tendonitis, tendinosis, tendinopathy, tendon tears, cartilage injuries)
• Hip: Labral tearing
o Impingement
o Psoas tendinitis
• Knee: Patellar tendonitis and tears
o Quadriceps tendonitis and tears
• Thigh/Buttocks: Hamstring strains
o Hamstring Tears
o Piriformis syndrome
o Ischiofemoral impingement
o Trochanteric Bursitis
• Elbow:
o Medial epicondylitis (golfer’s elbow)
o Lateral epicondylitis (tennis elbow)
• Shoulder: Rotator cuff tendonitis and partial tears
• Impingement
• Partial Rotator cuff tears
Acute and chronic ligament injuries (sprains)
• Elbow
• Hand
• Knee
• Hip
These therapies have been shown to be effective in treating osteoarthritis (OA). Arthritis is an inflammatory condition involving the breakdown of cartilage within a joint. Although it is still unproven as to whether PRP and Stem Cell treatment can be effective in re-growing lost cartilage or slowing cartilage breakdown, there is now evidence that these treatments are effective in treating the symptoms of arthritis. In fact, several new studies have shown that PRP is more effective than typical conservative treatments and has even performed better than viscosupplementation (hyaluronic acid injections) in head-to-head studies. Thus PRP may be an excellent non-invasive alternative to joint replacement surgery in treating the symptoms of arthritis. PRP can be used to treat the symptoms of arthritis of the shoulder, hip, knee, ankle and foot.
We would be happy to discuss the options available to you with respect to the difference between PRP and Stem Cells as well as the overall costs.